
Taylor Harrington, NICU Nurse.
This case study follows Chloe* (anonymised name), an infant born extremely pre-term who developed a volvulus and subsequent bowel ischemia resulting is a significant amount of small bowel to be resected.
Chloe was born at 23 weeks and 4 weeks gestation weighing only 535g. She has been intubated at birth and went on to require HFOV and Nitric Oxide. Chloe then received a postnatal course of dexamethasone and was extubated to CPAP on day 13 of life. At this time, she had been on full oral feeds of fortified expressed breastmilk via an orogastric tube.
Chloe has an acute deterioration on day of life 26 (corrected gestation 27 +2), requiring re-intubation, HFOV and nitric oxide. She had a grossly distended abdomen and abdominal films revealed dilated bowel loops but nil pneumotosis or free air. Chest film also showed bilateral consolidation consistent with pneumonia. She was started on antibiotics, placed nill by mouth and transferred to a tertiary NICU for an exploratory surgical intervention.
On arrival in NICU, Chloe was very unwell, and she was prepped for theatre. Due to her fragility and need for HFOV and Nitric Oxide, the theatre staff brought the operating room to Chloe and did a bedside laparotomy in NICU. The paediatric surgeons found a 720-degree midgut volvulus which was reduced and the bowel was found to be adequately perfused distal to the volvulus. The surgeons also performed a limited Ladd’s procedure. Chloe’s respiratory status immediately improved post op and her abdominal distention reduced. Her ventilation support was weaned as well as some of her inotropic blood pressure support.
In the next 24 hours, Chloe once again deteriorated. The NICU team had had increasing difficulty with her ventilation and further abdominal distention developed. Abdominal films were once again obtained and they revealed pneumatosis. The paediatric surgeons performed another bedside laparotomy where 45 cm of necrotic small bowel was resected. She had healthy bowel from the duodenojejunal flexure for 30 cm, then 45 cm of necrosis with 10 cm of distal ileum spared. A total of 40 cm of small bowel intact. Her ileocecal valve and colon were healthy. Chloe had a jejunostomy formed with an ileal mucous fistula.

She recovered well post operatively, but given the fact that she had a jejunostomy, she had very high, watery stoma output that looked milky. She was averaging losses of 40-60 ml/kg/day. This meant long term TPN for Chloe, but due to difficult IV access, central line infection risks and abnormal liver function tests the team tried to wean her off TPN quickly.
The neonatal team in collaboration with the neonatal dietician and pharmacist, trialled different formulas and anti-motility agents but they made negligible difference to her output. Chloe was struggling with growth and by five weeks post operatively at day 63 of age (32+6 weeks corrected) she had only gained 285 grams, an average of 7 grams/day. At this time, Chloe had a barium contrast test to check the patency of her distal bowel in the hopes that’s she was well enough to start trialling chyme reinfusion therapy.
Chloe was the first patient to ever use The Insides® Neo! Her parents consented to the trial the day of its approval. She was 63 days old (32+6) corrected, and coincidently her barium contrast results came back that same day so the surgical team cleared Chloe to commence chyme reinfusion therapy. At this time, she had been weaned off TPN, she was on continuous orogastric feeds in attempt to slow her output down and had very poor weight gain.
Chloe had already been fitted with the ‘Hollister Pouchkins Bag’ and required frequent stoma bag changes every 4-12 hours due to her high watery chyme output. With her next stoma bag change, the device was fitted and secured to Chloe. A size 6 Fr gastric tube was used for refeeding. It was inserted into the distal fistula to the 5cm marking and secured using the clip provided. The nursing team withdrew Chloe’s chyme every four to six hours and reinfused the chyme continuously over the next four to six hours via a syringe infusion pump. The neonatal team had concerns regarding the volume of chyme that was being reinfused, and it was agreed upon that if the distal stoma began to reflux the chyme back into the bag, the rate would be slowed down and it would have to be acceptable that she was only receiving partial volumes of chyme. To the NICU and surgical teams’ delight, she tolerated the whole volume of chyme being reinfused and had her first bowel motion in her nappy within 48 hours. Everyone was VERY excited, especially her family and The Insides® Company!

On day 77 of life (34+6 weeks corrected), Chloe continued to thrive with chyme reinfusion therapy. Chloe had been reinfusing for 14 days when the surgical team decided to perform a reanastomosis. This decision was made secondary to her high jejunal output. Chloe’s stoma output was consistently 60 ml/kg/day and although she was doing well with chyme reinfusion therapy, the hourly rate of reinfusion was very high, and she was starting to have some reflux from her distal stoma. In total, with 14 days of chyme reinfusion, Chloe gained 250g. That is 18g per day! Nearly two and a half times more weight gain than prior to starting chyme reinfusion therapy.
Chloe recovered well postoperatively and was on gut rest and full TPN for approximately one week before feeds were reintroduced. She transitioned well back to full feeds but continued to struggle with loose bowel motions and poor weight gain.
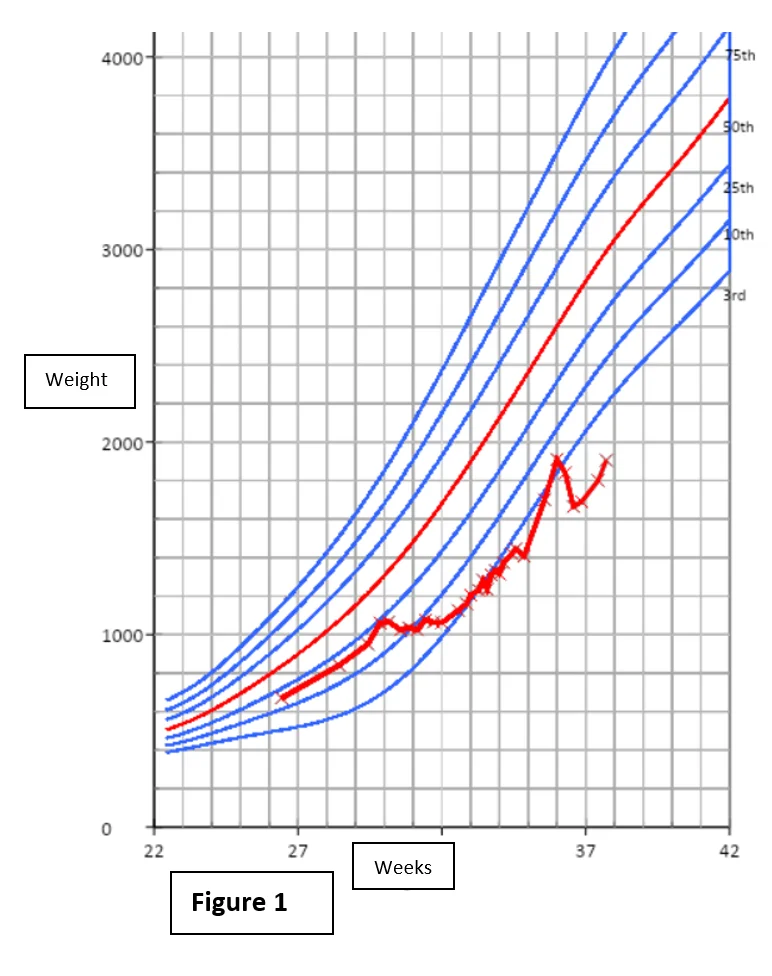
If you refer to Figure 1, you can clearly see from the date of her surgery, she had moderate weight gain until she was weaned off TPN, at 30 weeks corrected gestational age. She then had a period of static growth falling from the 25th centile to the 3rd. With the commencement of chyme reinfusion therapy at 32+6 weeks corrected gestation age, her static weight trend halted and she tracked along the 3rd centile nicely until her reanastomosis at 34+6 weeks corrected gestation age. After her reanastomosis, you can see a rapid weight gain postoperatively during the time she was on gut rest and full TPN. Once she was transitioned back to full oral feeds her weight once again dropped off, but she continued to make small gains and track upwards below the 3rd centile.
In conclusion, although the time that Chloe spent undergoing chyme reinfusion therapy via The Insides® Neo device was short, it was beneficial to her surgical recovery.
Chloe’s NICU journey was not an easy one for her or her family. Her stay was further complicated by a course of necrotising enterocolitis, which was managed medically with antibiotics and gut rest and no surgical intervention was required. She endured many of the typical challenges faced by infants born prematurely at 23 weeks gestation including chronic lung disease, retinopathy of prematurity, poor feeding and poor growth. Growth and feeding are things that that most premature babies struggle with, but Chloe even more so given her extensive surgical history.
Chloe spent a total of 200 days in Neonatal Intensive Care and was discharged home when she was 53 weeks corrected gestational age. She went home on a combination of high flow oxygen and low flow oxygen, saturation monitoring, apnoea monitoring, continuous nasogastric feeds and countless outpatient appointments.
Chloe is so fortunate to be surrounded by a family that loves and supports her through her journey. He parents were at her bedside every day even with a 1 hour commute each way. Her two big brothers were at home cheering her on as was evident by the artwork at her bedside. After a long journey, the whole family was excited to have her home where she has continued to thrive outside of a hospital setting.

Emma had an enteroatmospheric fistula form after being involved in a tragic car accident. She used The Insides System for close to 14 months, navigating her way through life as a 20 year old to successfully being reversed this year...

This case study follows Adrienne, a premature infant whose Neonatal Intensive Care stay was complicated by bowel perforations, significant faecal peritonitis and large volume turbid ascites, secondary to a milk curd obstruction. She required a beside laparotomy in the Neonatal Intensive Care Unit (NICU) and her postoperative journey was very difficult, complicated by hypovolemic shock, an aortic clot, a wound dehiscence with a fistula formation, and a further deterioration with septic shock leading to reduced blood flow to her small bowel.